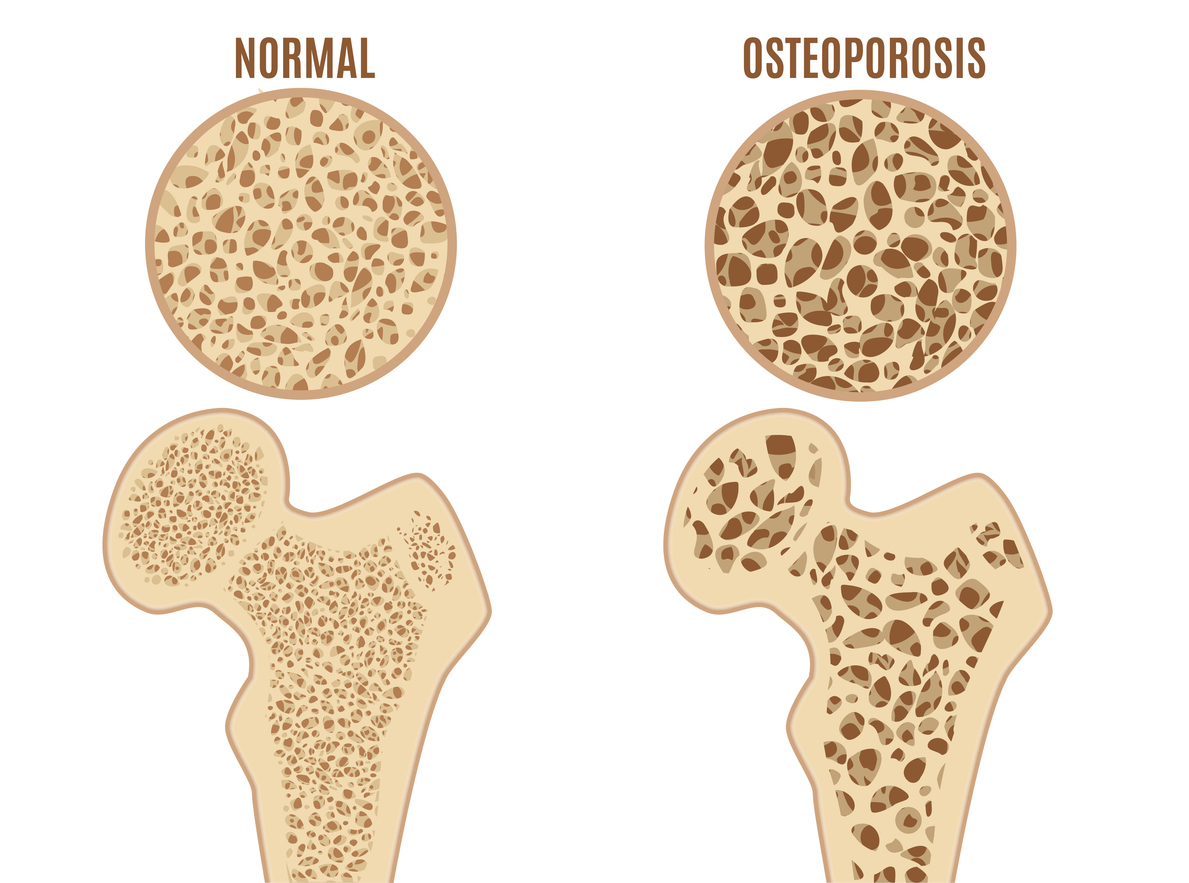
Osteoporosis is a condition that weakens bones, making them fragile and more likely to break. It’s a significant health concern, particularly as we age, but understanding the risk factors can help in its prevention. In this article, we’ll explore 3 risk factors of osteoporosis, shedding light on why some people are more prone to developing this condition than others. By identifying these risk factors—age, gender, and lifestyle choices—you can take proactive steps to protect your bone health. Whether you’re looking to prevent osteoporosis or manage it more effectively, knowing the risks is the first step toward stronger bones and a healthier future.

Age and Gender: The Unavoidable Risk Factors
Osteoporosis, often referred to as the “silent disease,” progressively weakens bones, making fractures more likely. Among the many risk factors, age and gender stand out as unavoidable influences that significantly impact bone health. Understanding how these factors contribute to osteoporosis can help in recognizing early warning signs and taking preventive measures.
Age: The Impact of Growing Older
One of the most prominent risk factors for osteoporosis is age. As we age, our bones naturally lose density and strength. This process typically accelerates after the age of 50, when bone mass decreases at a faster rate. The body’s ability to produce new bone diminishes over time, leading to a gradual loss of bone density. This makes older adults more susceptible to fractures, even from minor falls or injuries. The risk of developing osteoporosis increases with age, making regular bone density screenings crucial for early detection and management.
Gender: Why Women Are at Greater Risk
Gender also plays a critical role in osteoporosis risk. Women, particularly postmenopausal women, are at a higher risk than men. This increased vulnerability is largely due to the drop in estrogen levels that occurs during menopause. Estrogen is essential for maintaining bone density, and its decline can lead to rapid bone loss. In fact, women can lose up to 20% of their bone density in the first five to seven years after menopause. As a result, women are more likely to develop osteoporosis and suffer from fractures, particularly in the hip, spine, and wrist.

The Combined Effect of Age and Gender
When age and gender are combined, the risk of osteoporosis becomes even more pronounced. Older women are at the highest risk, especially those who experience early menopause or have a family history of osteoporosis. While these factors cannot be changed, being aware of them can encourage proactive steps, such as bone density tests, a calcium-rich diet, and weight-bearing exercises, to mitigate the risks.
By understanding these unavoidable risk factors, you can take early action to protect your bone health. Although age and gender cannot be altered, recognizing their impact on osteoporosis can empower you to make informed decisions about your health.
Genetics: How Family History Affects Bone Health
While age and gender are significant risk factors for osteoporosis, genetics also play a crucial role in determining your likelihood of developing the condition. If osteoporosis runs in your family, you may be at a higher risk, and understanding this connection can help you take preventive steps early on.
Inherited Risk: The Role of Genetics
Your genetic makeup can significantly influence your bone density and overall bone health. Studies have shown that having a parent or sibling with osteoporosis increases your risk of developing the disease. This is because genes control various aspects of bone formation, structure, and maintenance. For example, genetic variations can affect the body’s ability to absorb calcium, regulate hormones like estrogen, and build strong bones. If your family members have experienced fractures or have been diagnosed with osteoporosis, you might inherit these tendencies, making you more susceptible to bone loss and fractures.
Bone Health Across Generations
Bone health tends to follow patterns within families. If your parents or grandparents had osteoporosis, especially if they experienced fractures from minor falls, it’s essential to be proactive about your bone health. Genetic predisposition can make bones more fragile and less dense, even if you lead a healthy lifestyle. Understanding this inherited risk allows you to take steps such as getting early bone density tests, ensuring sufficient calcium and vitamin D intake, and engaging in weight-bearing exercises to strengthen your bones.
Combining Genetics with Lifestyle Factors
While genetics play a significant role, it’s important to remember that they are just one piece of the puzzle. Lifestyle choices can either mitigate or exacerbate your genetic risk. Even if you have a family history of osteoporosis, maintaining a healthy diet, staying active, and avoiding smoking and excessive alcohol can help reduce your risk. On the other hand, neglecting these aspects can make you more vulnerable, even if you don’t have a strong genetic predisposition.
By understanding the influence of genetics as one of the 3 risk factors of osteoporosis, you can take proactive measures to protect your bone health. Knowing your family history and combining that knowledge with healthy lifestyle choices can make a significant difference in preventing or managing osteoporosis.
Lifestyle Choices: Diet, Exercise, and Bone Density
While age, gender, and genetics are significant factors in osteoporosis risk, lifestyle choices also play a crucial role in bone health. The decisions you make regarding your diet, exercise, and other habits can either strengthen your bones or make them more vulnerable to osteoporosis. Understanding how these factors contribute to bone density is essential for preventing or managing the condition.
Diet: The Foundation of Strong Bones
A well-balanced diet rich in calcium and vitamin D is vital for maintaining bone density. Calcium is the primary building block of bones, and vitamin D helps your body absorb it effectively. Dairy products, leafy greens, and fortified foods are excellent sources of calcium, while sunlight exposure and foods like fatty fish provide vitamin D. However, poor dietary choices, such as consuming excessive amounts of processed foods, sugar, and caffeine, can negatively impact bone health. A diet lacking in essential nutrients can lead to weaker bones over time, increasing your risk of osteoporosis.
Exercise: Building and Maintaining Bone Strength
Physical activity is another critical factor in maintaining bone density. Weight-bearing exercises, such as walking, running, and resistance training, help stimulate bone growth and slow down the natural loss of bone mass that occurs with aging. Regular exercise also improves balance and coordination, reducing the risk of falls and fractures. On the other hand, a sedentary lifestyle can lead to muscle weakness and bone deterioration, making osteoporosis more likely. Incorporating regular exercise into your routine is one of the most effective ways to support bone health and reduce the risk of osteoporosis.
Avoiding Harmful Habits: Smoking and Alcohol
Certain lifestyle habits can also have a detrimental effect on bone health. Smoking has been shown to reduce bone mass and increase the risk of fractures, as it interferes with the body’s ability to absorb calcium and disrupts the balance of bone-remodeling hormones. Excessive alcohol consumption is another risk factor, as it can lead to bone loss and increase the likelihood of falls. Limiting or avoiding these harmful habits is essential for maintaining strong bones and reducing your osteoporosis risk.
By making informed lifestyle choices, you can significantly impact your bone health. While age, gender, and genetics are beyond your control, a healthy diet, regular exercise, and avoiding harmful habits are powerful tools in maintaining bone density and preventing osteoporosis. Understanding these lifestyle factors as one of the 3 risk factors of osteoporosis empowers you to take control of your bone health and reduce the risk of fractures as you age.
Summary
Osteoporosis is a condition influenced by multiple risk factors, including age, gender, genetics, and lifestyle choices. As people age, especially women after menopause, the likelihood of developing osteoporosis increases due to hormonal changes that lead to bone density loss. Genetics also play a significant role, as a family history of osteoporosis can predispose individuals to the condition. However, lifestyle choices such as a calcium-rich diet, regular weight-bearing exercise, and avoiding harmful habits like smoking and excessive alcohol consumption can help mitigate these risks. By understanding and addressing these 3 risk factors of osteoporosis, you can take proactive steps to maintain bone health and reduce the risk of fractures as you age.
The natural bone strength complex made from Satsuma mandarin orange
Juveriente®’s Bone Strength Complex is a natural supplement made from a traditional dietary habit of a healthy bone town in Japan. People there eat a lot of Satsuma mandarin orange and have high concentration of Beta-Cryptoxanthin, a kind of carotenoid. A cohort study there found that that concentration has high reverse correlation with onset ratio of osteoporosis.
It provides you the essence of a natural food, which is simply an extract of a Japanese popular citrus fruit. It is according to your principal policy. Needless to say, it is better to try a natural food before jumping to strong medicines. Though natural and gentle, it has garnered a lot of amazing reviews in Amazon since its launching in 2016.
If you like to try multi-vitamin supplement, how about adding the natural bone therapy fruit extract with Juveriente® Bone Strength Complex?
Please learn details in our product page.